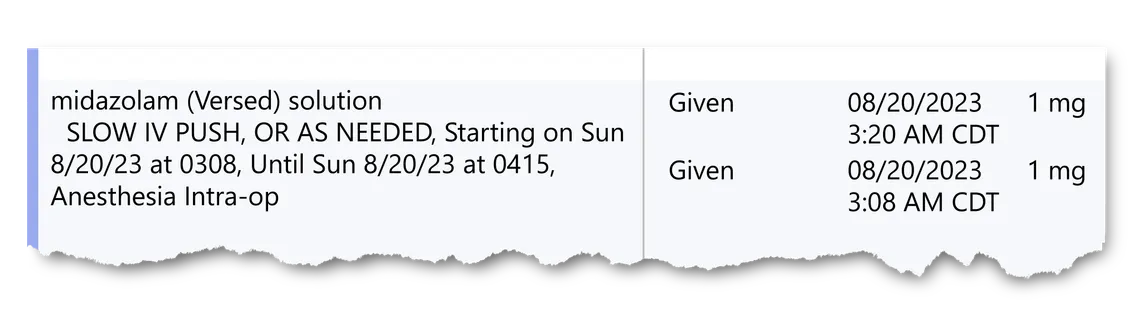
Amairani Salinas was 32 weeks pregnant with her fourth child in 2023 when doctors at a Texas hospital discovered that her baby no longer had a heartbeat. As they prepped her for an emergency cesarean section, they gave her midazolam, a benzodiazepine commonly prescribed to keep patients calm. A day later, the grieving mother was cradling her stillborn daughter when a social worker stopped by her room to deliver another devastating blow: Salinas was being reported to child welfare authorities. A drug test had turned up traces of benzodiazepine — the very medication that staff had administered before wheeling her into surgery.
For Victoria Villanueva, pregnant with her first child, the drug detected in her baby’s system was morphine. Villanueva had arrived at an Indiana hospital at 41 weeks to have her labor induced. To ease the pain of her contractions, doctors gave her narcotics. A day later, a social worker told the new mother: The baby’s meconium — or first bowel movement — had tested positive for opiates. Now, instead of bonding with her baby, Villanueva shook with fear that her newborn could be taken away. “I didn’t even know how to function,” she recalled.
What happened to Salinas and Villanueva are far from isolated incidents. Across the country, hospitals are dispensing medications to patients in labor, only to report them to child welfare authorities when they or their newborns test positive for those very same substances on subsequent drug tests, an investigation by The Marshall Project and Reveal has found.
The positive tests are triggered by medications routinely prescribed to millions of birthing patients in the U.S. every year. The drugs include morphine or fentanyl for epidurals or other pain relief, anxiety medications, and two different blood pressure meds prescribed for C-sections.
In a time of increasing surveillance and criminalization of pregnant women since the end of Roe v. Wade, the hospital reports have prompted calls to the police, child welfare investigations and even the removal of children from their parents.
The reporting for this story included interviews with two dozen patients and medical professionals, and a review of hundreds of pages of medical and court records. Some spoke about cases on condition of anonymity because the custody of children is at stake.
In New York, a mother with no history of drug use lost custody of her toddler and newborn for five months after she tested positive for fentanyl that the hospital had given her in her epidural. In Oklahoma, when a mother tested positive for meth, sheriff’s deputies removed her newborn and three other children. They were held in foster care for 11 days, until a confirmation test proved that the culprit was a heartburn medication the hospital had given the patient.
By the time of Villanueva’s hospital stay in 2017, researchers and doctors had known for years that medications can rapidly pass from mother to baby, causing positive drug test results. Two tests from Villanueva’s prenatal visits, and another test done right before she went into labor, all showed the mother had no drugs in her system. The morphine given to Villanueva for her contractions was documented in her medical records. But the staff reported her to the state child welfare agency anyway, hospital records show.
Marion General Hospital in Indiana did not respond to requests for comment. Brian Heinemann, a spokesperson for the Indiana Department of Child Services, declined to comment on Villanueva’s case, but said policy has since changed to ensure that drug screen results alone are not used to substantiate an allegation of abuse or neglect.
Kimberly Walton, a spokesperson for the Texas Health Resources system, declined to answer questions about Salinas’ case, but said that doctors order drug tests if there is a concern about patient health, and that they are required “to report suspected illegal drug use that could endanger the health or safety of a child.”
Hospital drug testing of pregnant women, which began in the 1980s and spread rapidly during the opioid epidemic, was intended in part to help identify babies who might experience withdrawal symptoms and need extra medical care. Federal law requires hospitals to alert child welfare agencies anytime such babies are born. But a previous investigation by The Marshall Project and Reveal found that the relatively inexpensive, pee-in-a-cup tests favored by many hospitals are highly susceptible to false positives, errors and misinterpretation — and many hospitals have failed to put in place safeguards that would protect patients from being reported over faulty test results.
In some cases examined by The Marshall Project, doctors and social workers did not review patient medications to find the cause of a positive test. In others, providers suspected a medication they prescribed could be the culprit, but reported patients to authorities anyway.
“How much harm to birthing people are we willing to allow? Our patients are being harmed until we can get our act together,” said Dr. Davida Schiff, whose hospital network, Mass General Brigham in New England, instituted a new policy this year that directs providers to drug test patients, with their consent, only when medically necessary. The new policy also halted automatic reporting of positive test results. Hospitals have a responsibility to address the testing problems, she said. “The hospitals are at fault. The clinicians are at fault. Our policies are at fault.”
The risks from giving medications to birthing patients and then testing them for illicit substances have been well documented. A 2022 study by researchers at Massachusetts General Hospital found that 91% of women given fentanyl in their epidurals tested positive for it afterward. Other studies have found that mothers can quickly pass these medications onto their babies. A baby’s positive drug test “cannot and should not be used to identify fentanyl drug abuse in mothers,” said Athena Petrides, the lead researcher of one of the studies at Brigham and Women’s Hospital in Boston.
Despite these warnings, hospitals often lack policies requiring providers to review a patient’s records to see what medications they received before reporting them to authorities. Mandatory reporting laws protect doctors from liability for reports made “in good faith,” even if they turn out to be wrong. And toxicologists and doctors say many doctors lack the time and expertise needed to adequately interpret drug test results.
“It’s not something routinely taught in medical school or even residency,” said Dr. Tricia Wright, an OB-GYN and professor at University of California, San Francisco Medical Center who specializes in substance use disorders in pregnancy. “It’s all up to individuals who make their own interpretations.” Wright helped change the policy at her hospital, one of the country’s leading teaching facilities, to direct doctors not to drug test patients unless medically necessary.
While drug tests can help pediatricians determine how to treat an infant who may experience withdrawal symptoms, many OB-GYNs say that positive drug test results do not generally inform the mother’s medical care, so they have little reason to dwell on them.
Instead, at many hospitals, it is social workers — responsible for contacting child welfare agencies — who are more likely to pay attention to drug test results. Some hospitals require social workers to automatically file a report for any positive test, while other facilities first perform an assessment to determine whether a parent might be a risk to the baby.
But hospital social workers are often overworked, said Kylie Haines, who manages a program for pregnant women with opioid use disorder at Vanderbilt University Medical Center, one of the top maternity teaching hospitals in the nation. Social workers generally have even less training than doctors on drug testing, and little authority to question test results, she said. Investigating the cause of a positive drug test is not considered part of their job.
“We’re not medical providers,” said Haines, a licensed social worker herself. “We can’t interpret drug screens.”
The timing of the tests can also make it tricky to interpret them. In theory, the best time to take a urine sample for drug testing is when a patient arrives at the hospital, before receiving medications. But it is common for hospitals to test urine samples taken from a birthing patient’s catheter bag, or to request a urine sample after medications have already been administered, providers said.
Newborn drug tests can add another layer of complexity. While urine tests can detect potential drug use over a period of days, testing the baby’s meconium can uncover illicit substances going back months. Meconium tests are widely considered to be the gold standard for newborn drug testing because they can indicate potential drug use earlier in pregnancy, a possible sign of addiction.
But in some cases, there is no way to tell whether a baby’s positive test was caused by a medication the hospital dispensed or a substance the mother used earlier. Nor do such tests tell providers how much or how frequently a person may have used drugs — for example, if a patient used substances in the past but stopped when she realized she was pregnant. “You actually don’t know,” said Schiff. “Which is kind of a mess.”
Medications such as morphine or fentanyl have led some patients to get flagged as opioid users. Ephedrine and phenylephrine, medications for low blood pressure that are commonly prescribed during C-sections, have caused false positives for meth. The Marshall Project also found that women were questioned over positive drug tests after hospitals gave them sedatives such as benzodiazepines or barbiturates.
When women are flagged by a positive drug test result, other aspects of their lives can quickly come under suspicion. Medical conditions or birth complications that can be associated with addiction — such as high blood pressure, a placenta that separates before birth or a premature birth — may mistakenly be viewed as further evidence that a pregnant patient used drugs. Through the lens of a positive drug test, even something as innocuous as missing some prenatal appointments becomes potential evidence that a mother is a risk to her baby. And patients who had traumatic experiences giving birth may suddenly find themselves under threat.
In 2023, Salinas was still in a haze of grief after delivering her stillborn baby when she learned she would be reported to child welfare authorities. Salinas had no idea the hospital had given her the benzodiazepine for which she tested positive and denied using the medication. She had also tested positive for Delta-9, a legal hemp-derived product, which she said she had bought at the grocery store. But soon, Salinas found herself under a monthslong investigation, trying to fight off paralyzing depression while processing her grief and caring for her other children.
“I still have three live children. They still need to eat. They still need to get up for school. They still need their mom,” Salinas recalled thinking as she was being questioned.
Officials closed the case about four months later as “unsubstantiated.” But it wasn’t until a year later that Salinas read through her medical records with a Marshall Project reporter and discovered the cause of the positive test.
Marissa Gonzales, a spokesperson for the Texas Department of Family and Protective Services, declined to discuss Salinas’ case, citing confidentiality laws.
Salinas said she wondered why child welfare workers weren’t spending their time investigating allegations of actual child abuse. “Why are you giving your attention to this person who’s a good mom, who hasn’t done anything, instead of a child who may actually be in danger?”
In recent years, studies have found that drug tests aren't necessarily the best way to identify someone with a substance use problem — a simple screening questionnaire is also effective. Leading medical groups advise hospitals to use questionnaires instead of universal drug tests. But hospital drug testing — and reporting — of labor and delivery patients remains ubiquitous.
In at least 27 states, hospitals are required by law to alert child welfare agencies about a positive test or a potential exposure to the baby. But not a single state requires hospitals to confirm test results before reporting them. Hospitals routinely contact authorities without ordering confirmation tests or waiting to receive the results.
Not every state explicitly requires reporting a positive test, but many hospitals do so anyway. In 2022 alone, more than 35,000 babies were reported to child welfare authorities as substance-exposed, federal data shows, with no guarantee that the underlying test results were accurate.
“The system is primed for a report,” said Dr. Mishka Terplan, an OB-GYN in Maryland and a leading researcher on substance use disorders during pregnancy. “To slow it down, or to stop it, takes effort.”
The consequences of a faulty drug test can be especially severe for people with histories of addiction, who are less likely to be believed when they protest that the positive test was caused by a hospital medication. In this environment, a patient’s word is often pitted against a single drug test, and it’s up to an individual doctor, nurse or social worker to decide whether to ferret out the truth.
Lisa Grisham, a nurse in Arizona, recalled the case of a patient in recovery for opioid use disorder who tested positive for fentanyl. The woman insisted that another nurse had given her the medication during labor, even though it was not listed in her hospital records. Grisham, the director of a hospital program for substance-exposed infants at Banner University Medical Center in Tucson, took it upon herself to investigate and eventually tracked down the nurse, who confirmed the patient’s explanation.
“It makes me sick to think of all the moms that have come through and said they don't use fentanyl and we don’t believe them,” Grisham said.
Villanueva was just 18, newly married and still working on her GED when she gave birth to her first baby. As a child, she had been taught to be honest with medical providers. So during hospital admission, she told a nurse that she had briefly experimented with drugs such as marijuana and acid when she was 15 years old. She hadn’t used drugs since, she said.
When she was admitted, Villanueva took a drug test that came back negative for any illicit substances — the same result as the two drug tests from her prenatal appointments. Then she received medicine to induce labor, and her contractions began. They were so painful, Villanueva recalled, that she was relieved when a nurse told her she was giving her morphine.
The day after Villanueva gave birth, an investigator with the Indiana Department of Child Services arrived. The hospital had informed the agency about Villanueva’s “history of drug use,” according to medical records. Without her knowledge, Villanueva said, the hospital also sent her daughter’s meconium for testing, which found the morphine.
Villanueva was certain that her hospital records would prove she had received morphine, and she was right. The drug test results even stated, “Drugs administered during labor and delivery may be detected in meconium.”
But even after the investigator received the hospital records, Villanueva said, the agency required her to submit to more drug tests and allow inspections of her home. Finally, after several weeks, the agency closed the case, Villanueva recalled.
Only after the investigators were out of her life did Villanueva feel that she could finally revel in her baby’s birth and allow herself to be happy.
“I couldn’t even really enjoy properly my child being born,” she recalled. “Until after the fact, when they were gone.”